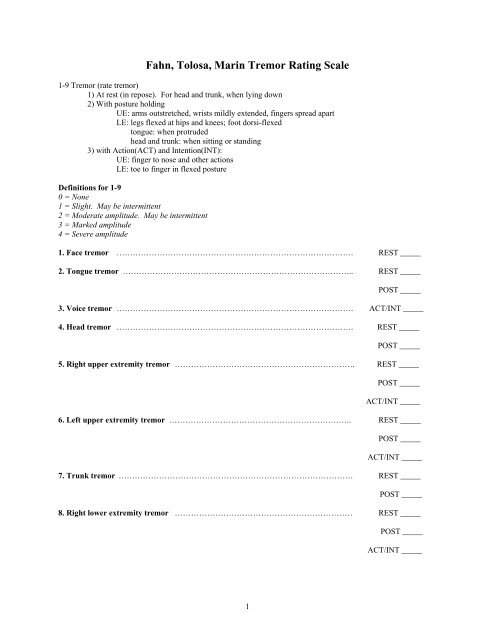
Background: The Fahn-Tolosa-Marin Clinical Rating Scale for Tremor (FTM) has been used in large trials for essential tremor (ET), but its anchors for ratings from 0 to 4 of upper limb tremor are probably too low for patients with severe tremor (tremor amplitude >4 cm; grade 4). TETRAS has a 12-item activities of daily living (ADL) subscale that addresses many of the activities assessed in the ADL scales of Fahn, 6 Louis, 11 Bain, 7 and their coworkers, and TETRAS also has a 9-item performance subscale that quantifies tremor in the head, face, voice, limbs and trunk.
Competing Interests: The authors of this manuscript have the following competing interests: R.B. Dewey, III, BS reports no disclosures. O’Suilleabhain, MD reports grants from AVID. Sanghera, PhD reports no disclosures. Patel, MD reports grants from Adamas. Khemani, MD reports advisory boards with Lundbeck, honoraria from Lundbeck and Dallas School of Neuroscience and Sleep Medicine, and grants from NIH and Once Upon a Time Foundation. Lacritz, PhD reports advisory boards with Teva, honoraria from Omni hotel, John Peter Smith hospital, and Parkland hospital, and grants from NIH/NIA neurobiology of aging and the State of Texas, Texas Alzheimer's Research and Care Consortium.
Chitnis, MD, PhD reports consultancies with Teva and Medtronic, advisory boards with Teva, honoraria from Teva, and grants from Teva, Medtronic, NIH, and Allergan. Whitworth, MD reports no disclosures. Dewey, Jr., MD reports consultancies with Teva, Acadia and Impax, advisory boards with Teva, Acadia, Lundbeck and Impax, honoraria from Teva, Acadia, Impax, Merz, US WorldMeds, Lundbeck, and UCB, and grants from NIH. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Results The result of this quality improvement process was the development of a neuromodulation network. The key aspect of this program is rigorous patient assessment of both motor and non-motor outcomes tracked longitudinally using a REDCap database. We describe how this information is used to identify problems and to initiate Plan-Do-Study-Act cycles to address them. Preliminary outcomes data is presented for the cohort of PD and ET patients who have received surgery since the creation of the neuromodulation network. Introduction Treatment of disorders such as PD, ET, and dystonia requires an individualized, multi-faceted approach consisting of non-pharmacological therapy, medications, and surgical treatments. Currently, high frequency deep brain stimulation (DBS) is the most commonly recommended surgical approach when response to medication is inadequate [, ].
DBS consists of an implantable neurostimulation system that creates a non-destructive and reversible disruption of the abnormal activity in the basal ganglia or thalamus to improve motor symptoms [, ]. Selection of the target is based on disease specific considerations including the patient’s most disabling symptoms, as well as co-morbid cognitive and mood symptoms. Adobe flash cs3 free trial. Once the system is implanted the device is programmed to deliver electrical current to the targeted area.
Randomized trials of DBS in PD report a range of outcomes. A recent review tabulated the results of a number of studies of both STN and GPi DBS []. Of the 9 studies reporting on 943 patients undergoing STN DBS, the mean improvement in UPDRS III scores and PDQ-39 index scores ranged from 29–49% and 8.3–26.4% respectively.  The same outcome measures for GPi DBS performed in 377 patients showed mean improvements of 29–39% and 6.3–17.5%. Possible reasons for a variable response, even at pioneering hospitals where pains have been taken to optimize the processes, include patient differences such as anatomy and physiology at the millimeter scale and operational differences such as the trajectory planning process and the heuristics used to decide a lead location is good enough to quit searching for better.
The same outcome measures for GPi DBS performed in 377 patients showed mean improvements of 29–39% and 6.3–17.5%. Possible reasons for a variable response, even at pioneering hospitals where pains have been taken to optimize the processes, include patient differences such as anatomy and physiology at the millimeter scale and operational differences such as the trajectory planning process and the heuristics used to decide a lead location is good enough to quit searching for better.
During the early years of our DBS practice, we followed published guidelines on patient selection, surgical technique, and post-operative programming, but there was no systematic collection and review of the outcomes, so there was a missed opportunity to learn based on performance. In the course of routine clinical care we discovered 2 cases of suboptimal clinical responses to DBS, and post-operative imaging confirmed that the leads were not optimally located. These findings prompted a closer look at our DBS program, leading to a quality improvement initiative to refine patient selection, imaging, surgery, and post-operative programming to achieve more consistently positive outcomes.